Regulation of Kidney Function
Enroll to start learning
You’ve not yet enrolled in this course. Please enroll for free to listen to audio lessons, classroom podcasts and take practice test.
Interactive Audio Lesson
Listen to a student-teacher conversation explaining the topic in a relatable way.
Osmoreceptors and ADH Release
🔒 Unlock Audio Lesson
Sign up and enroll to listen to this audio lesson

Today, we are going to discuss the role of osmoreceptors in kidney function. When there's a loss of fluids, these receptors activate, prompting the hypothalamus to release antidiuretic hormone, also known as ADH. Can anyone tell me what ADH does?

ADH helps reabsorb more water in the kidneys?

Exactly! ADH facilitates water reabsorption in the distal convoluted tubule and collecting duct. This reduces urine output. Remember the phrase 'ADH makes you retain that H2O!' Can anyone tell me why this is important?

It's crucial for regulating blood pressure and fluid balance!

Correct! This helps prevent dehydration and maintains blood volume. Wonderful discussion! Let's move on to the next topic, the JGA.
Juxtaglomerular Apparatus (JGA)
🔒 Unlock Audio Lesson
Sign up and enroll to listen to this audio lesson

The JGA is crucial in the regulation of kidney function. It detects changes in blood flow and pressure. What happens when blood flow decreases?

The JGA releases renin, right?

Correct! Renin initiates the renin-angiotensin mechanism. Can someone explain what this mechanism does?

It converts angiotensinogen to angiotensin I and then to angiotensin II, which increases blood pressure!

Exactly! Angiotensin II is a potent vasoconstrictor. It raises GFR and stimulates aldosterone release for sodium and water reabsorption. Remember the acronym 'RAAS' - Renin, Angiotensin, Aldosterone System - to help you remember these key concepts!
Atrial Natriuretic Factor (ANF) and Regulation Balance
🔒 Unlock Audio Lesson
Sign up and enroll to listen to this audio lesson

We’ve talked a lot about hormones like ADH and the renin-angiotensin mechanism. Let’s discuss Atrial Natriuretic Factor or ANF. What role does ANF play?

ANF opposes the effects of aldosterone and renin, right?

Exactly! ANF is released when there's increased blood volume and pressure, leading to vasodilation and decreased blood pressure. How does this counteract the renin-angiotensin system?

It helps keep blood pressure from getting too high by causing vasodilation!

Well done! This balance between ANF and the renin-angiotensin mechanism is crucial for maintaining homeostasis in our bodies!
Introduction & Overview
Read summaries of the section's main ideas at different levels of detail.
Quick Overview
Standard
Kidney function regulation involves complex feedback mechanisms that include the hypothalamus, the JGA, and hormonal responses to changes in blood volume and pressure. Key hormones like antidiuretic hormone (ADH) and aldosterone play significant roles in controlling water reabsorption and blood pressure.
Detailed
Regulation of Kidney Function
The kidneys perform a vital role in maintaining homeostasis by regulating fluid balance, electrolyte levels, and blood pressure. This regulation is achieved through intricate hormonal feedback mechanisms primarily involving the hypothalamus, the juxtaglomerular apparatus (JGA), and the heart.
Key Points Covered in this Section:
-
Osmoreceptors Activation:
Osmoreceptors in response to changes in blood volume and ionic concentration trigger a hormonal response. When fluid loss is excessive, the hypothalamus releases antidiuretic hormone (ADH) from the neurohypophysis. - Role of Antidiuretic Hormone (ADH):
- Function: ADH facilitates water reabsorption in the tubules, which helps prevent excess urination (diuresis).
- Blood Pressure Effect: ADH also has vasoconstrictive properties that can increase blood pressure, leading to increased renal blood flow and elevated glomerular filtration rate (GFR).
- Juxtaglomerular Apparatus (JGA):
- Function of JGA: The JGA, located where the distal convoluted tubule contacts the afferent arteriole, senses decreases in GFR or plasma flow.
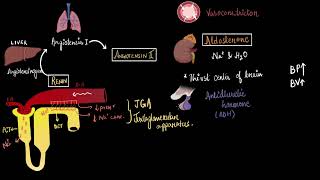
- Renin-Angiotensin Mechanism: A fall in blood flow triggers the JGA to release renin. Renin catalyzes the conversion of angiotensinogen to angiotensin I and then to angiotensin II, a potent vasoconstrictor that increases GFR and blood pressure.
- Aldosterone Release: Angiotensin II stimulates the adrenal cortex to secrete aldosterone, leading to sodium and water reabsorption in the distal tubules, further increasing blood pressure.
- Atrial Natriuretic Factor (ANF):
- Counteracting Mechanism: ANF is released in response to increased blood flow to the heart's atria, causing vasodilation, decreased blood pressure, and counteracting the renin-angiotensin mechanism.
In conclusion, the regulation of kidney function is a complex interplay of hormones that ensure the body's fluid and electrolyte homeostasis is maintained effectively.
Youtube Videos

Audio Book
Dive deep into the subject with an immersive audiobook experience.
Hormonal Feedback Mechanisms
Chapter 1 of 6
🔒 Unlock Audio Chapter
Sign up and enroll to access the full audio experience
Chapter Content
The functioning of the kidneys is efficiently monitored and regulated by hormonal feedback mechanisms involving the hypothalamus, JGA and to a certain extent, the heart.
Detailed Explanation
The kidneys are crucial organs that maintain the body's internal environment. Their function is regulated by hormones, mainly through a feedback system controlled by several organs including the hypothalamus and the juxtaglomerular apparatus (JGA) located in the kidneys themselves. This means that the body detects changes in fluid levels and blood pressure and adjusts kidney function accordingly to maintain balance.
Examples & Analogies
Think of the kidneys as a thermostat in your home. When the temperature goes too high or too low, the thermostat detects this change and activates the heating or cooling system to maintain a comfortable temperature. Similarly, when the body experiences changes in blood volume or pressure, the kidneys adjust their functioning through hormonal signals to keep our internal environment stable.
Role of Osmoreceptors and ADH
Chapter 2 of 6
🔒 Unlock Audio Chapter
Sign up and enroll to access the full audio experience
Chapter Content
Osmoreceptors in the body are activated by changes in blood volume, body fluid volume and ionic concentration. An excessive loss of fluid from the body can activate these receptors which stimulate the hypothalamus to release antidiuretic hormone (ADH) or vasopressin from the neurohypophysis. ADH facilitates water reabsorption from latter parts of the tubule, thereby preventing diuresis.
Detailed Explanation
Osmoreceptors are specialized cells that detect the concentration of electrolytes in the blood. When the body loses water (like during heavy sweating), these receptors signal the hypothalamus to release ADH. This hormone tells the kidneys to retain more water, reducing the amount of urine produced. This process helps maintain fluid balance in the body, especially in dehydrating conditions.
Examples & Analogies
Imagine working outside on a hot day and sweating a lot. Your body needs to conserve water to avoid dehydration. Just as you would drink more water or seek shade to avoid losing too much water, your body uses ADH to tell the kidneys to keep more water and lessen urine output, so you stay hydrated.
Feedback Mechanism with Blood Volume
Chapter 3 of 6
🔒 Unlock Audio Chapter
Sign up and enroll to access the full audio experience
Chapter Content
An increase in body fluid volume can switch off the osmoreceptors and suppress the ADH release to complete the feedback. ADH can also affect the kidney function by its constrictory effects on blood vessels. This causes an increase in blood pressure. An increase in blood pressure can increase the glomerular blood flow and thereby the GFR.
Detailed Explanation
When the body has enough fluid, the osmoreceptors stop sending signals, leading to a decrease in ADH production. This means that the kidneys will release more water, resulting in more urine and reducing blood volume back to normal. Additionally, ADH causes blood vessels to constrict, increasing blood pressure, which can further enhance blood flow to the kidneys and improve filtration rate.
Examples & Analogies
Consider a water tank in your house. When the tank is full, a float switch stops the water supply. If the tank starts to empty, the switch tells the supply to refill it. In the same way, a full body reduces ADH, allowing the kidneys to expel excess water, similar to releasing water from the tank!
Juxtaglomerular Apparatus and Renin
Chapter 4 of 6
🔒 Unlock Audio Chapter
Sign up and enroll to access the full audio experience
Chapter Content
The JGA plays a complex regulatory role. A fall in glomerular blood flow/glomerular blood pressure/GFR can activate the JG cells to release renin which converts angiotensinogen in blood to angiotensin I and further to angiotensin II.
Detailed Explanation
The JGA is a specialized area in the kidneys that senses changes in blood pressure. If blood flow drops, the JGA releases an enzyme called renin. Renin triggers a cascade that produces angiotensin II, a powerful vasoconstrictor that raises blood pressure and helps restore blood flow in the kidneys, thereby enabling them to maintain proper function.
Examples & Analogies
Imagine an employee (renin) being called in when a team's performance is dropping (blood pressure decreases). This employee has the power to suggest important changes that improve the team's overall efficiency, just like renin triggers responses that help stabilize kidney function.
Aldosterone Action
Chapter 5 of 6
🔒 Unlock Audio Chapter
Sign up and enroll to access the full audio experience
Chapter Content
Angiotensin II, being a powerful vasoconstrictor, increases the glomerular blood pressure and thereby GFR. Angiotensin II also activates the adrenal cortex to release Aldosterone. Aldosterone causes reabsorption of Na+ and water from the distal parts of the tubule. This also leads to an increase in blood pressure and GFR.
Detailed Explanation
Aldosterone, a hormone released due to signals from angiotensin II, promotes reabsorption of sodium ions and water in the kidneys. This process increases blood volume and blood pressure, which in turn helps the kidneys to filter more blood, maintaining an effective glomerular filtration rate.
Examples & Analogies
Think of the kidneys like a sponge soaking up water. When you add more power (sodium and water retention) to the sponge, it absorbs more fluid increasing the overall capacity and pressure in the system. This is how aldosterone helps the kidneys retain water and maintain proper blood pressure and filtration rate.
Role of Atrial Natriuretic Factor (ANF)
Chapter 6 of 6
🔒 Unlock Audio Chapter
Sign up and enroll to access the full audio experience
Chapter Content
An increase in blood flow to the atria of the heart can cause the release of Atrial Natriuretic Factor (ANF). ANF can cause vasodilation (dilation of blood vessels) and thereby decrease the blood pressure. ANF mechanism, therefore, acts as a check on the renin-angiotensin mechanism.
Detailed Explanation
When blood volume increases, the heart releases ANF, which dilates blood vessels, lowering blood pressure. This process counteracts the effects of the renin-angiotensin mechanism, helping to prevent excessive blood pressure increases and ensuring that kidney function remains balanced.
Examples & Analogies
Think of ANF as the emergency brake in a car. If the car is going too fast (high blood pressure), pulling the emergency brake (release of ANF) slows the vehicle down by relieving some pressure. This ensures a safe and controlled operation, just like ANF regulates blood pressure to keep kidney functions steady and efficient.
Key Concepts
-
Osmoreceptors: Sensory receptors that activate hormonal responses to maintain fluid balance.
-
ADH: Hormone that assists in water reabsorption in the kidneys.
-
JGA: Structure that regulates GFR and blood pressure through the renin-angiotensin system.
-
Renin: Enzyme released by JGA that initiates the production of angiotensin II.
-
ANF: Hormone released by the heart that counteracts high blood pressure.
Examples & Applications
ADH release in response to dehydration, increasing water reabsorption in the kidneys.
The renin-angiotensin mechanism where low blood pressure leads to increased renal blood flow and GFR.
Memory Aids
Interactive tools to help you remember key concepts
Rhymes
ADH helps you stay hydrated, without it, your trips to the loo are elevated!
Stories
Imagine your body as a city, and the kidneys as water controllers; when the city starts to run dry (dehydration), the main controller (hypothalamus) sends a urgent message (ADH) to keep as much water as possible inside to keep the city thriving.
Memory Tools
Remember the mnemonic 'RAAS' - Renin, Angiotensin, Aldosterone System to understand the cascade of events when blood pressure drops.
Acronyms
To remember the roles of ANF, think 'ANF = A Natural Fluid reducer' since it counters blood pressure.
Flash Cards
Glossary
- Osmoreceptors
Sensory receptors that detect changes in osmotic pressure in the body.
- Antidiuretic Hormone (ADH)
A hormone that promotes water reabsorption in the kidneys and helps regulate blood pressure.
- Juxtaglomerular Apparatus (JGA)
A structure in the nephron that helps regulate blood pressure and glomerular filtration rate by releasing renin.
- Renin
An enzyme released by the JGA that converts angiotensinogen into angiotensin I.
- Angiotensin II
The active form of angiotensin that causes blood vessel constriction and increases blood pressure.
- Atrial Natriuretic Factor (ANF)
A hormone released from the heart that reduces blood pressure by causing vasodilation.
- Homeostasis
The maintenance of stable internal conditions within an organism.
Reference links
Supplementary resources to enhance your learning experience.
